
Healthcare Insights : Why Are Doctors Organizing?
By John August
While the actual numbers of attending physicians organizing unions is relatively small, the increase in activity is significant.
In my view this data vastly underestimates the activity among doctors to reclaim their voice and power as a profession.
We should consider two other important facts which tells us that doctors demand for organization is much greater than the data shows:
- The phones are “ringing off the hook” at the nation’s dominant healthcare unions SEIU, AFT, and AFSCME. The unions have the experience, the will, and the resources to respond. The phones are also “ringing off the hook” at the professional organizations that represent doctors, including the AMA, state medical societies, and the myriad professional organizations which represent the many specialties in medicine. These organizations are trying to catch up to the demands coming from their members to provide information and support for the demand to organize.
Additionally, public officials and the media are reporting new and startling events regarding physician organizing as well:
On February 13, 2025, the Boston City Council unanimously passed a resolution in support of 300+ primary care doctors to organize at one of the nation’s largest and most prestigious institutions: Massachusetts General/Brigham.
Earlier this month a 27-day strike by physician hospitalists at Providence Health in Oregon was settled on issues of pay and reformed staffing models.
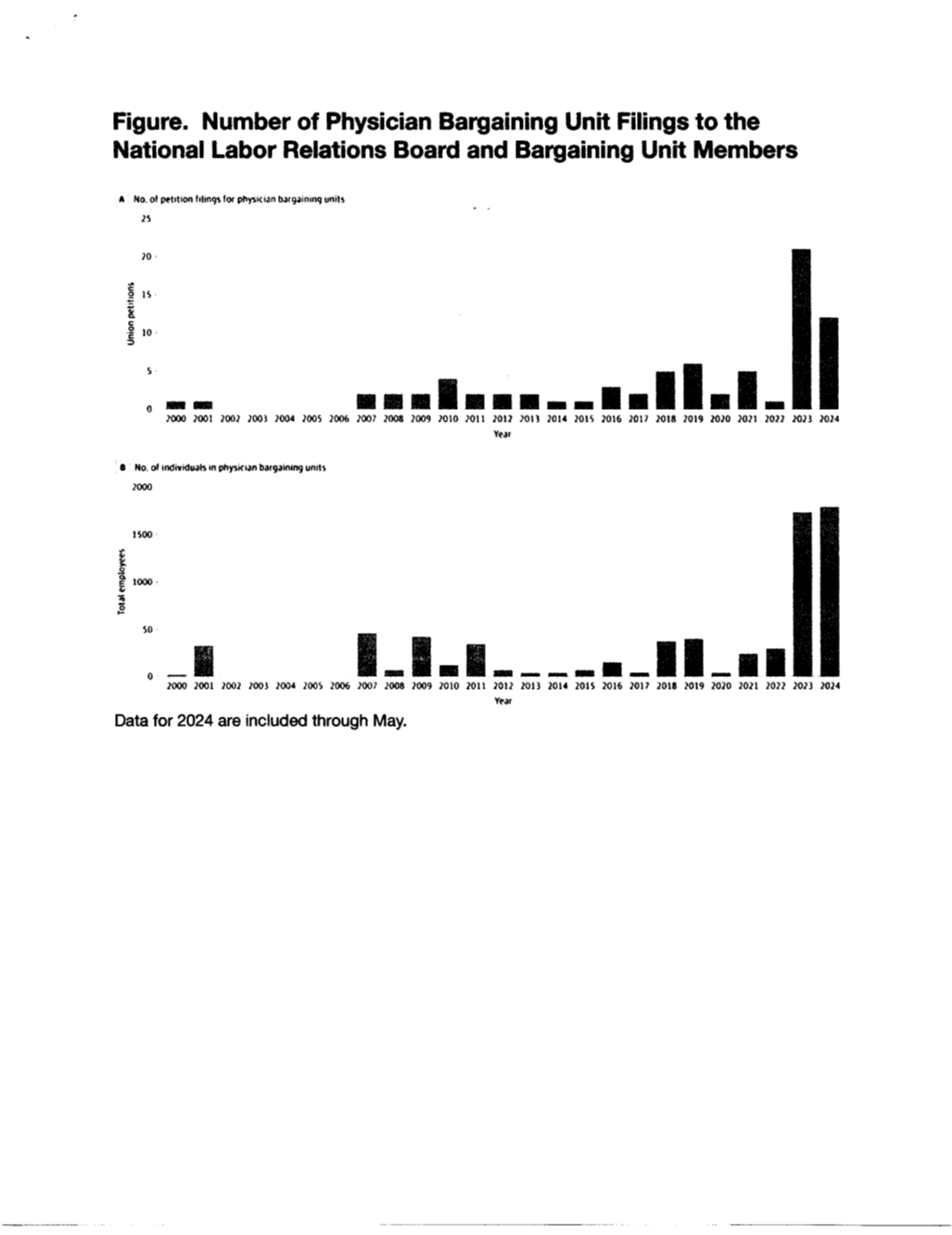
The charts below taken from the Journal of the American Medical Association’s December, 2024 research paper on physician unionization, illustrate a huge increase in traditional union organizing has occurred among the nation’s attending physicians. (This research focuses on attending doctors, NOT interns and residents).
The lead in the article states: “Declining morale and increased corporate employment have led many physicians to consider unionization.”
In several articles in this column, I have discussed the increase in union activity among attending doctors. I have reported on union election victories and the issues in those campaigns. I have discussed the rapid growth of the consolidation of the industry and the evidence that these consolidations have not resulted in the promise of improved access, improved care, and lower costs. In fact, these trends have resulted in the opposite.
It seems that the central motivation for unprecedented interest among the nation’s doctors is the extraordinary confluence of two major shifts: Today 75% of doctors are employed by a corporate entity as the industry is consolidating into larger and larger systems. As newly employed physicians, they have lost autonomy and long-standing control over their practice. Through most of our history, doctors worked in individual or group practices, able to maintain their autonomy over decisions about patient care. That control is disappearing.
In this month’s edition of Healthcare Insights, I will share the views of an advocate and leader for physician unionization, Dr. Lauren Beene, a pediatrician from Cleveland, Ohio. She shared with me the multi-level motivations of doctors to organize to regain their voice and power over:
- Day-to-day barriers to their ability to practice medicine as they were trained to do,
- The sanctity of the physician-patient relationship,
- The many systemic dysfunctions in the health system itself which are at the core of the moral injury that doctors experience by losing control over their practice,
- Social and ethical issues in health and healthcare in the community’s physicians serve, and nationally.

Before I share her observations and insights, it is very important to remember how we arrived at this moment in the history of physician experience.
The traditional status of physicians as independent practitioners lasted through many decades of debate in the United States about the need for healthcare reform: for far too long, too many of our people have had limited access to care; costs are higher than anywhere else in the industrialized world, while the health of our population ranks at the bottom of that cohort of nations.
Mostly driven by the Centers for Medicare and Medicaid (CMS), the federal agency which both pays for and regulates payments to hospitals and doctors for the majority of services performed in U.S. healthcare, there has been a slow but steady shift from traditional fee-for-service-medicine to fees for outcomes for patients as a central strategy to improve care. This shift often reduces payments for individual patients
One major result of this shift has been a rapid consolidation of health services into larger and larger systems in a failing effort to use size and scale to offset the pressure to provide improved care with less revenue per patient.
This pressure also drove many independent and group practices of doctors to consolidate or more recently to be taken over by either large health systems or private insurance companies. It has been through this process that doctors have had their employment status shift from independent practitioner to employee.
It seems that the pendulum of power and decision-making has swung all the way to the side of large health systems, including for-profit systems, and an overall trend toward corporate medicine. Corporate medicine is defined broadly as the trend in which medical decisions are taken out of the hands of individual doctors and instead, fall to the commercial or corporate entities where care is provided. More and more, these large systems are the employers of the doctors who as a result are losing their professional autonomy.
In her own words, Lauren Beene, MD, is a dedicated community pediatrician committed to providing the highest quality care to all patients without barriers. She co-founded Ohio Physicians for Reproductive Rights, which led the successful 2023 initiative to enshrine reproductive freedom in Ohio’s Constitution. Dr. Beene earned her degrees from Cornell University, Oakland University, and Case Western Reserve University School of Medicine, and completed her training at Rainbow Babies & Children’s Hospital, where she served as chief resident. She is the proud mother of two incredible daughters who inspire everything she does.
Dr, Beene is leading the organization of 2,000 physicians at University Hospitals in Cleveland, Ohio.
I had the privilege of interviewing Dr. Beene for this article. I began the interview with this question: “Why are doctors organizing, and specifically can you address this phenomenon in the context of day-to-day experience of doctors?”
It turned out that was the only question I needed to ask. In a free-flowing set of personal reflections, Dr. Beene articulated an inspiring vision of why the day-to-day experience of medical practice cannot be separate from larger social and political dynamics of health and healthcare. In this vision, she explains why physicians are organizing.
Dr. Beene grew up in Flint, Michigan, well aware of the famous autoworker sit down strike that established the UAW. She said she herself did not come from a union family but was influenced personally by that history.
She became a pediatrician and saw herself as an advocate for children as individuals and as part of the community.
When the Dobbs decision struck down Roe v. Wade, she immediately realized that patients were going to suffer, especially the poor and people of color who always bear the brunt of these policies most. She felt as though she did not have a voice in this crisis but went to a Women’s Physicians Facebook Page and commented on the crisis that was to come from Dobbs. A doctor named Marcela Azevedo saw Dr. Beene’s post and reached out. Together, they asked for doctors to sign a letter opposing Dobbs, and within a couple of days more than 1000 doctors signed onto the letter. She pointed out that this was a very risky thing for doctors to do.
Dr. Beene and her colleagues, asked for support from their medical societies, from health systems, and other professional associations which they did not receive.
They pushed ahead.
The doctors published the letter in the Columbus Dispatch which asked to support a ballot initiative on Reproductive Freedom.
The doctors formed Ohio Physicians for Reproductive Rights which led the campaign to have the initiative put on the ballot in 2023. At the polls the initiative passed by a 57-43 margin guaranteeing a Constitutional Right to all reproductive care in the State of Ohio.
From that experience, Dr. Beene learned the art of organizing. She read posts on a Physicians’ Moms Facebook page which included participation from 80,000 women doctors. This is where Dr. Beene started hearing about and learning about physicians’ unions.
Dr. Beene shared with me her experience of medical education and early practice. She started medical school in 2010 and residency in 2015 at Rainbow Babies, one of the most important children’s hospitals in the nation. She described Rainbow as a leader in cystic fibrosis research and practice, in the development of pediatric multi-specialty clinics, and among the first hospitals to allow parents to room with their children when they received treatments and surgeries.
She loved the environment of care, she loved her mentors, and knew it was the only place she wanted to practice medicine.
But she noticed that many of the attending physicians who trained her and whom she admired were leaving the hospital and going to work elsewhere. These doctors were leaving because they saw an erosion of the standards that had kept them there.
She witnesses and heard from her colleagues about:
- Loss of control over the physician-patient relationship
- Reduction of time allowed with each patient
- Micro-managing of practice and protocols
- Top-down decision making
- Inability to provide safe care
- Nurses and other support staff were also leaving which meant that more non-physician duties were falling on physicians
- There was a confusing management of available resources
Dr. Beene considered what seemed obvious to her: The doctors generated all the revenue for the health system, yet when issues of financial stress evolved, decisions were made to acquire or build new facilities with no transparency of these decisions. Patient care continued to erode.
A doctor contacted her and inquired if she had thought about unionization and she immediately recognized that without power the erosion of conditions would continue. She also realized that no one was going to confer power on doctors, but that they would have to use the legal system to stop the health system from making unilateral decisions not in the interest of patients and physicians.
I listened intently to Dr. Beene’s articulate and multilayered response to my original question: why are doctors organizing?
What I learned from her is that doctors see themselves as advocates for their patients. From the scientific method they use for diagnosis, to the broad knowledge base they develop from decades of training and patient engagement, to the relationship of the individual patient conditions to broader social and political root causes of disease and injury, all these dynamics and more define advocacy as doing the best for each individual, while learning that the advocacy is compromised by not having power to advocate for structural reform and improvement to make care and outcomes better.
To bring color and specificity to how advocacy is eroded in today’s environment of corporate decision making in healthcare, I share a few brief additional stories from other doctors. The names of the doctors are withheld as well as the location of care to protect the doctors, and not to compromise any confidentiality of medical information:
- An oncologist discussed what happened after there was a large layoff of mostly supportive providers about a year ago, including multiple oncology, nurse coordinators. The oncologist lost the luxury of having nurses who could connect with patients and ensure that patients with newly diagnosed cancer had appointments with the right physicians as soon as possible and that the right studies were being done in a timely manner. Without the nurse managers that were laid off, this oncologist finds herself having patients inappropriately scheduled to see her which often causes a delay in the appropriate care.
- Another doctor has certifications in OB GYN, maternal fetal medicine, and genetics. She is responsible for the ultrasounds performed on women who have been found to have high risk pregnancies such as fetal malformations. The administration of the clinic insists that she sees 55-65 patients per day, a number that is outrageous in any specialty. This doctor has to do the ultrasound, diagnose a complex and likely rare genetic condition, and then have a meaningful conversation with scared parents.
- There was also the case of the doctor who expressed a chronic feeling of exhaustion because of a lack of control over his schedule.
- Yet one more doctor stressed: “A few years ago, when they brought on a couple more docs and did not pay for anymore medical assistants, I was told that the medical assistants would only do blood pressure and weight at follow up visits. They would not have time to review meds and allergies. Medications and allergies were only going to be reviewed at new patient visits. At the same time, I was told I could review it myself but that they wanted me to decrease my visit time from 40 to 30 minutes. So, they took away my time with the patients and gave me more to do. They felt it was not medically necessary to check meds and allergies at every visit. (And the person telling me this was a physician!!!!!)”
De. Beene’s story and some of these other specific experiences of doctors highlighted in this month’s column illuminates what is causing the increase in physician organizing. More importantly, I think it is fair to say that a movement of doctors to find the right models of organization is underway. My sense is that physicians are uniquely positioned to claim power through organization and as they do create new forms of organization with scale and speed.
John August is the Scheinman Institute’s Director of Healthcare and Partner Programs. His expertise in healthcare and labor relations spans 40 years. John previously served as the Executive Director of the Coalition of Kaiser Permanente Unions from April 2006 until July 2013. With revenues of 88 billion dollars and over 300,000 employees, Kaiser is one of the largest healthcare plans in the US. While serving as Executive Director of the Coalition, John was the co-chair of the Labor-Management Partnership at Kaiser Permanente, the largest, most complex, and most successful labor-management partnership in U.S. history. He also led the Coalition as chief negotiator in three successful rounds of National Bargaining in 2008, 2010, and 2012 on behalf of 100,000 members of the Coalition.
