
The Collaboration Council of the North Central Bronx Hospital
A Strategic Initiative Between Doctors Council SEIU and New York City Health + Hospitals by Samantha Na and John August
The Little Hospital Who Could
We are all living through the greatest challenge in a century to the health and well-being of all. Perhaps as never before, the shortcomings of not just our health care systems, but of our social infrastructure as a whole have been exposed in ways expected and unexpected.
To be frank, the shortcomings have been in place for a long time. We all demand systemic solutions, and sooner than later.
It is also the case that the healthcare workforce goes to work each day with the intent of not just doing the best it can under the circumstances, but to do the very best for patients, for the community, and for themselves.
This brief study of the New York City Health + Hospitals/ North Central Bronx Hospital (NCB) Collaboration Council has been undertaken because it is but one example of what is possible…what is possible based on trusting relationships driven by collaborative efforts to solve real problems for real people no matter the circumstances. The collaborative efforts are rooted in data-driven inquiry, use of scientific methods, and dedication to the achievement of demonstrable, data-driven improved outcomes for patients.
There are similar efforts going on among their colleagues across the largest public health system in the nation in which nearly every non-managerial employee belongs to a union. This mobilization of collaborative problem solving ought to be part of that equitable and effective social infrastructure that we must achieve.
We believe that shining a light on “The Little Hospital Who Could” is inspiring, but more importantly essential for all to learn from. The dedicated staff have achieved so much with so little. So often in the world that is the way so much progress is actually made.
Doctors Council SEIU is the largest Union of attending doctors in the nation, with members located in New York City, New Jersey, Pennsylvania, and Illinois. Its largest constituency works in the nation’s largest public health system, the New York City Health and Hospitals Corporation (NYC H+H), serving 1.4 million predominantly poor New Yorkers who constitute a high percentage of the immigrant population of the City. Like public health all across the nation, NYC H+H faces enormous financial challenges while maintaining its mission to provide care to all who need it regardless of ability to pay or immigration status.
In 2015, Doctors Council and NYC H+H agreed to a new provision in their collective bargaining agreement: to establish both a system-wide and facility- based Collaboration Councils in all 21 of the System’s facilities. The Collaboration Councils were designed to increase patient experience and doctor engagement. (see attached collective bargaining agreement provision in the Appendix).
The Collaboration Councils have grown in impact and effectiveness since first launched in 2016. The Councils represent efforts rooted in the collective bargaining relationship, emphasizing improvement in the experience of the patients. The improvement effort is driven by frontline doctors and other staff alongside facility- based leadership.
“It is critically important to understand how difficult it is in the U.S. for labor and management to evolve to a collective bargaining relationship that reflects the world around them in ways that are beneficial to them and to the communities in which they live. After decades of transformation of the economic, social, demographic, public policy, technological, financial, and competitive landscape, for collective bargaining to remain relevant, it must also transform.” [i]
The Collaboration Councils represent a unique ongoing experiment in a patient centered collective bargaining framework.
This brief study of the NCB Collaboration Council provides a window into the system-wide effort by the Union and the Health System to create a sustainable foundation to achieve goals of improvement in patient experience and doctor engagement.
All NYC H+H facilities and communities they serve share most of the financial, demographic, and organizational characteristics of NCB, including the challenges to build and sustain successful Collaboration Councils. NCB was chosen for this study because of its unique character as the smallest of the system’s acute care hospitals. And like its counterparts across the City of New York in the public hospital system, it operates each day in the framework of limited resources.
The doctors at NCB often refer to their hospital as “the little hospital who could,” or more recently during the height of the COVID-19 pandemic as “the People’s Hospital.”
An Overview/Framework
This brief paper showcases the smallest acute care facility in the largest public health system in the nation. Why is this of interest and importance?
Collective bargaining in the United States faces a period of great challenge and opportunity. With only 11-12% of the U.S. workforce belonging to Unions today as compared with 35% in the 1950s, the relative strength, influence, and purpose of collective bargaining are in focus…it is a time of creative and transformative reflection about the forms and features that it should take.
The Collaboration Councils, established by the Doctors Council and the NYC H+H system, represent a large experiment in collective bargaining outcomes. The North Central Bronx Collaboration Council is a part of that experiment.
We believe there are several important frames in which to explore and evaluate the importance of the Collaboration Councils broadly and specifically at North Central Bronx:
1.) Public health in the United States is under-resourced
“While the United States spends an estimated $3.6 trillion annually on health, less than 3 percent of that spending is directed toward public health and prevention. Furthermore, public health spending as a proportion of total health spending has been decreasing since 2000 and falling in inflation-adjusted terms since the Great Recession. Health departments across the country are battling 21st-century health threats with 20th- century resources. The COVID-19 crisis demonstrates this reality in the starkest of terms. [ii]
While all of the NYC H+H facilities face similar challenges, NCB tends to stand out because of its small size and location in one of the nation’s poorest neighborhoods. As such, our colleagues in Doctors Council and NYC H +H agree that NCB is a wonderful example to showcase what is possible!
We are reminded of the work of Dr. Jeffrey Brenner. He came to prominence working as a primary care doctor in Camden, NJ in the early 2010s. His passion was to identify the city’s most vulnerable patients and connect them through his primary care practice to hospitals that could treat them for largely preventable chronic conditions. To accomplish this effort, he set up a practice inside one of Camden’s poorest housing projects and made his services available to people who would otherwise have no access to primary care.
For the kickoff talk for the Aspen Institute Public Health Grand Rounds lecture series, Dr. Jeffrey Brenner, a 2013 MacArthur Fellow, explained how he used ‘health care hotspotting’ to identify the reasons for high costs in Camden, New Jersey. Brenner, a family physician and executive director of the Camden Coalition of Healthcare Providers, defines hotspotting as “using data sets to find outliers, with the idea that outliers are often the canary in the coal mine,” said Brenner. “Outliers will tell you the failures of a complex adaptive system.”
“A small sliver of patients is responsible for much of the costs, but we really ignore them,” said Brenner.
For one case study, Brenner described an outlier patient who had nine emergency room visits, six admissions to the hospital, 12 medications a day, and several severe medical conditions, including kidney failure and cancer. By looking into this case, Brenner revealed that one main reason for the high cost of care is because the various medical departments treating this patient and others are disjointed and are not trained to collaborate with each other.
“When asked at a conference about his success against such enormous odds, Dr. Brenner answered that “I learned that it is those who have the least funds who often make the largest breakthroughs.”
This is the kind of thinking that drives our interest in NCB!
2.) The Essentiality of Collaboration to system success
“In the current social and political landscape, we hear much more about polarization than we hear about trust. Yet at the same time, there is a substantial if not a majoritarian view that the nation must achieve a version of a social compact in which all members of society expect that their vulnerability to social pressures ought to be reduced and that we have a responsibility to one another to live safe, productive, healthy lives in a sustainably built system.” [iii]
Let us consider a particular kind of workplace: a “collaborative community”.[iv] The authors of the article referenced here advance the idea that through the development of collaborative communities at work through building blocks (see below), sustainability can be achieved.
▪ Building a sense of shared purpose
▪ Cultivating an ethic of contribution
▪ Developing processes that enable people to work together in flexible but disciplined projects
▪ Creating a collaborative infrastructure
From healthcare to education, to manufacturing, and public employment, to all sectors of the economy, we believe it is fair to ask: what kinds of organizational structures are we building that will be successful not just as enterprises, but as collaborative communities where all participants realize in their daily lives that the shared purpose in work is to create the conditions for a new social compact? And I think we can agree that without trust, such a social compact cannot be achieved.” [v]
The Collaboration Councils were established to foster improved doctor engagement and patient experience. Whether the goal is to improve communications between frontline doctors and executives, whether the goal is to improve various drivers of patient experience and health outcomes, the Collaboration Councils serve as a problem-solving forum. As such, they provide a building block of a collaborative community, one which fosters trust among participants and within the organization.
Finally, the doctors of the Doctors Council recognized that they needed to create a new structure in order to effectively and sustainably contribute to improving the outcomes for patients. The Collaboration Councils constitute a new and necessary organizational structure not found in the current structures alone: the administration, the Union, or even the union contract. Please see the Appendix attached, “NCB Quality Improvement Training”, developed through the Collaboration Council at NCB.”
This training illustrates much more than training: it represents a call for an entirely new approach to engaging the doctors!
3.) Continuous Learning
Over the past five years, all of the NYC H + H facilities have formed Collaboration Councils. The Collaborations Councils have advanced strategic capabilities. This unique joint labor-management effort will answer some of our great challenges that exist:
● How does a large health system that is challenged financially, with rising expectations of patients and the broader public that supports the system, improve its performance?
● How does the union continue to engage members above and beyond traditional bargaining, and grievances to help improve patient care and the public health system as a whole?
As part of the strategic improvement path of care and services, the FBCC’s focuses on an essential element of that strategy: enhanced physician engagement. The creation of a collaborative, learning environment that contributes to strategic patient-focused improvement is a strategy attempted by many health systems. We also know that one of the largest challenges across the industry is the ability to engage physicians and other healthcare workers. “In Towers Watson’s most recent global workforce study, less than half (44%) of the U.S. hospital workforce overall was highly engaged. That leaves a large proportion of employees across all workforce segments feeling somewhat disconnected from their hospital system and its goals and unsupported to some extent in doing their jobs well.” [vi]
Doctors Council and NYC H+H recognized that many approaches could be undertaken to create sustained engagement of the staff, which is so critical to achieving sustained improvement in care and patient experience. The parties have chosen a strategy that is founded on a commitment to the creation of a learning environment.
“Research has shown that teams whose leaders explicitly framed implementation as a learning rather than as a performance challenge were more likely to abandon existing interpersonal routines, including those premised on hierarchical interactions, and to adopt collaborative learning behaviors (Edmondson, 2003). Moreover, members of these teams (regardless of professional rank) felt psychologically safe and excited about offering their input.
Additionally, research has shown that individuals and teams that adopt a learning frame display less risk aversion, experiment more, persist longer with the task, learn more, and ultimately perform better than those who apply a performance frame (Dweck & Leggett, 1988; Edmondson, 2003). These observations suggest that HCOs (health care organizations) should explicitly frame innovation implementation as a learning challenge. This frame effectively minimizes both the perceived interpersonal and task- based risk of implementation.”[vii]
The Community of North Central Bronx
Recently, NCB has merged into the operational oversight by the much larger NYC Health and Hospitals/Jacobi Medical Center. And for many decades, “little NCB” has functioned in the shadow of one of NYC’s most iconic hospitals, Montefiore Medical Center. Nonetheless, NCB’s unique location and profile remain one of New York’s hidden gems.
North Central Bronx Hospital is composed of low to middle-income communities, consisting of many immigrant families. Although a predominantly Hispanic population, many Bangladeshis, Ecuadoreans, Guyanese, and Jamaicans are members of the hospital as well. 42% of patients identify as Hispanic or Latino, 32% as Black Non-Hispanic, and 7% as Asian or Other Pacific Islander. The top patient languages requested are Spanish, Bengali, Arabic, and Albanian, with 26% of people in the area speaking another language at home. 64% of hospital patients are female, while 36% are male. NCB serves a younger patient group, compared to that group’s proportion in the Bronx, with 24% of patients are under the age of 21, 36% ages 21-44, 29% ages 45-64, and 11% are aged 65 and older.
There are many green spaces and access to community gardens to exercise, as well as affordable housing in the neighborhoods. However, many NCB members report a downward trend in the neighborhood, with a concern for noise and air pollution, alcohol and drug use, homelessness, and a lack of healthy grocery stores. The Bronx Norwood community is located in Fordham-Bronx Park Area with service areas that include Crotona/Tremont, Fordham/Bronx Park, Highbridge/Morrisania, Kingsbridge/Riverdale, and Northeast Bronx. The zip codes include 10467, 10468, 10458, 10466, and 10457 where 50% of the patients reside. Many of the areas have populations below the 100% federal poverty level, Non-US citizens, less than high school education, live with a disability, high average jail rates, and speak English “less than well.”
53% of those seeking acute care services at NCB met NY State Medicaid eligibility guidelines with low eligibility thresholds for low-income individuals and families. There is a disproportionate share of services for the borough’s low-income and uninsured population with 67% of its inpatient discharges that were uninsured or enrolled in Medicaid, compared to 51% at Voluntary hospitals. NCB's mission statement is to provide high-quality healthcare, regardless of ability to pay and seeks to provide for the community.[viii]
NCB provides many services that include adult medicine/surgical, children’s, women’s health, and behavioral health care. Many patients seek services in routine well and preventative care, dental, hypertension, and complications in pregnancy.
North Central Bronx hospital’s COVID intensive care unit opened on May 5, 2020 that doubled its capacity. NCB took patients from other public and private hospitals, utilizing temporary ICU units in make-shift areas. The Bronx area had one of the highest numbers of COVID cases per head of population in the city, ranking third in the number of positive cases of any county across New York. Many of the neighborhood residents are more likely to work in frontline jobs; have underlying chronic medical conditions; they lack personal protective gear and paid sick leave, and they live in overcrowded conditions, making it difficult to quarantine safely.
NCB's 20-bed temporary ICU unit was a major step in providing care in the community, and by May 2020 NCB had a total of 215 beds and a rapid expansion of 120 additional ICU beds to help manage the surge of COVID patients. NCB was nicknamed “The People’s Hospital.” Many hospital members came together to step up, especially in an overflow of patients received from other hospitals during this time.[ix]
NCB, like its counterpart hospitals in NYC Health +Hospitals across the City, has many opportunities and challenges. Here are some specific opportunities and challenges that NCB faces:
● Its community health ranking is 62nd out of 62 counties in New York State
● High rates of diabetes, stress, challenged emotional well-being, heart disease, and high blood pressure
● Lack of adequate affordable high-quality housing
● High incidence of drug use, including opioids
● Obesity and high BMI
● Asthma
● Mental health disorders including depression
The maternity service of North Central Bronx hospital includes a natural childbirth service that has offered groundbreaking maternal and infant outcomes. North Central’s obstetric program started in 1977, and the survival for infants continuously outranks the average for both city’s municipal hospitals and general service deliveries. Midwives are co-managed with obstetricians to care for prenatal, intrapartum, and postpartum for all mothers. The hospital has a cesarean rate of 11.8 percent, one of the lowest rates in New York City.[x] The NCB is one of the only hospitals where mothers can give birth without drugs or anesthetics that negatively affect the infant. The NCB midwives not only help provide care during pregnancy that allows for ease of labor and delivery, they provide birth control and treat gynecological disorders both before and after pregnancy.
Many residents, hospital workers, and community leaders protested the absence of a birthing center when the unit was temporarily shut down due to staff shortages in 2013. The Unit reopened with support from the community in 2014. NCB undertook a renovation of the unit, modernizing and reconfiguring its delivery units and bed recovery wing to improve patient experience and access to Women’s health services. The renovation of the Midwifery unit allows patients to have access to gynecological and obstetric services and labor and delivery services all on the same floor.
The Collaboration Councils and the Facility Based Collaboration Council at NCB
The Facility Based Collaboration Councils (FBCC) were launched jointly by Doctors Council and NYC H+ H in February, 2016. The NCB FBCC was one of the first to achieve consistent success. Its original leaders included:
Balvindar Sareen MD, FACHE, Chief Medical Officer
Maureen Pode, Chief Executive Officer, co-lead
Jana Romm, MD, Doctors Council co-lead
Josephine, Sullivan, MD., Dentistry
Frederick Nagel, MD, Adult Emergency Department
Michael Packman, MD, Ambulatory Medicine
Helene Hordines, MD, Ophthalmology
Mayanne Marra, CNO
Christina Contreras, COO
The Collaboration Councils are standing committees of joint facility-based leadership in each of New York City Health and Hospitals’ institutions. They are composed of the executives and chiefs of the institution, and frontline attending physicians and dentists. In many cases, department heads of nursing and ancillary services and Performance Improvement advisors attend the councils. They meet monthly, charged with the following responsibilities:
● Improve communication between the administration and the union doctors about the strategic plan of NYC H + H at a system and facility-based level and how the frontline clinicians can best contribute to the system’s success;
● Improve the engagement of frontline clinicians in the qualitative improvement of the system and of the facility in which they work;
● Identify joint patient-focused improvement projects which serve as a means to build a learning environment for continuous improvement of the clinical quality and experience of the patients our system serves;
Pursuant to the collectively bargained Memorandum of Agreement, here is a summary of the commitments, operating guidelines, and goals of the Collaboration Councils:
• “There will be established a first- ever System-wide Joint Steering Committee. It will be composed of one Doctors Council member representative from each of 21 facilities in the HHC system and top HHC management, including the Chief Medical Officer, Chief Operating Officer, the SVP of Affiliations, the Chief Quality Improvement Officer, and the Chief Financial Officer. The role of the Joint Steering Committee will be to oversee the successful implementation of facility-based high priority quality joint patient care improvement initiatives designed to attain strategic and sustainable improvements in the delivery of health care to our patients. We hope to convene the first meeting in November 2015.”
• Three months after the System-Wide Joint Steering Committee has been meeting, there also will be established Facility-based joint committees at each of 21 facilities in HHC. The facility- based committees will be composed of one Doctors Council member from each department, as well as management representatives similar to those on the Steering Committee from the respective facility (COO, CMO, CFO, and CQO). These committees will convene 90 days after the first Steering Committee meeting.
• Doctors Council will be recruiting for both the System-Wide Joint Steering Committee and the Facility-based committees concurrently to establish unity of involvement and purpose across the system.
The Scope of the Collaboration Councils is broad: they are designed to create effective sponsorship and effective environments in the following areas:
• Improved overall patient experience
• Improved clinician engagement
• Improved access to HHC services
• Improved care coordination, prevention, patient education, and communication
• Improved clinician recruitment and retention
• Improved stewardship of HHC resources
• Improved development and use of "metrics that matter"
• Improved communication
Enablement of success will be achieved by:
• Joint development of "demonstration projects" as learning laboratories
• Creation of safe environments for learning and problem-solving
• Development of educational programs to enhance knowledge and engagement of clinicians, paying close attention to the changing healthcare landscape, healthcare reform, business literacy, and quality measures
NCB began its FBCC efforts early and successfully
One of the first projects at NCB evolved organically through discussions at the Facility- Based Collaboration council meetings. Staff conveyed a consensus that a major problem to be solved in the hospital was the inefficient patient registration process in the pediatric Emergency Department.
The Council sponsored “walk-throughs” of the registration process that encouraged staff to take on the registration experience of a patient. Through this experience, staff began to identify choke points and barriers. Prior to starting the root cause analysis, most staff thought it would be impossible to improve this central experience of the patient.
After more than two weeks of observation and evaluation of the problems, Dr. Daran Kaufman, the Director of Pediatric Emergency Medicine at the time sat with staff and recorded their observations. From these observations, the IHI Model of Improvement was utilized:
Initial Aim Statement:
1) Improved Patient Experience / Satisfaction:
a. Decrease median Wait time (arrival to provider) to 30 minutes within 3 months. Improve the patient experience by not requiring patients to move to seven different stations in order complete registration
2) Decrease the number of patients that leave without being seen to .5% within 3 months
The FBCC engaged doctors, nurses, registration clerks, and PCAs about their concerns and perceived barriers to a more efficient patient flow:
They identified the following problems to solve:
1) Delays in patient care due to long, inefficient registration process.
2) Delays in care leading to disgruntled patients
After a round of engagement with staff, the FBCC refined the initial AIM statement:
NEW AIM: What we are trying to accomplish:
1. Improved Patient Experience / Satisfaction:
- Decrease median Length of Stay to 75 minutes within 3 months
- Decrease median Wait time (arrival to provider) to 30 minutes within 3 months
- Improve the patient experience by not requiring patients to move to seven different stations in order complete registration
- Decrease the number of patients that leave without being seen
Doctor’s Engagement was central to the success of the project:
1. Developed PDSA cycles, worked with interdisciplinary team, and communicated plans and cycles to all staff.
2. Two weeks following implementation, one on one meetings with each physician and AHP to discuss their recommendations/ concerns.
3. Metrics shared on PI boards in ED.
4. Executive Administration met regularly with physicians, AHP and nurses for feedback and encouragement.
Improvements derived from this initial project at NCB included:
● Patients enter the Pediatric ED and are placed into a treatment room where they are seen immediately by the registration clerk, the triage nurse, and the treating provider.
● Wait time from door to provider for discharged patient: 1 hour six minutes to 35 minutes
● Wait time from triage to see first provider: 48 minutes to 21 minutes
● Length of stay for discharged patients: 1 hour 42 minutes to 1 hour 15 minutes
● Left ER without being seen: 3% to 0.9%
● Overall Press Ganey score on satisfaction 50 to 99
● Overall Press Ganey score on wait time 43 to 88
At the time of the end of this first project in 2018, Dr. Sareen, the CMO stated: “We all know that NCB is resource poor, but if you want something to change and get it done, ask someone who is already busy and they will find the time”, he said. “NCB has always had a fighting spirit.”
Dr. Kaufman indicated that with the success of this project and the learning that came with it, an effort to make similar improvements in Adult ER registration took off and paved the way for a successful future for the FBCC.
Prior to the start of the pandemic, the Executive Director at North Central Bronx at that time, Cristina Contreras made the following observation about the Collaboration Council:
“It is a cornerstone of the multifaceted approach to expanding the provision of quality of care to our patients. Our providers volunteer their time to partner with administration to create initiatives and track their progress, moving the needle on the delivery of safe, quality healthcare. It is this spirit of service and commitment to improving the health of their patients that inspires others to continue to work to enhance the delivery of care. Doctors give so much of themselves to be able to care for patients, and they take on that responsibility as a calling. The doctors in the Collaborative Council take that calling a further step, and work together to ensure the care they deliver as efficient and safe as possible.” –Cristina Contreras, Executive Director***(as of this writing, Ms. Contreras has taken on the leadership role of CEO at Metropolitan Hospital, another large NYC H+H facility. The current CEO is Christopher Mastromano who is the CEO of Jacobi Medical Center. NCB has been just recently merged with Jacobi.)
The experience of the FBCC at NCB was summarized this way by one of its co-leads: “The FBCC is an important resource at North Central Bronx Hospital. It gives front line providers a chance to work with executive leadership to achieve real and tangible change. Projects to date have improved the already excellent care that we give our patients, while at the same time improving patient and provider satisfaction. I appreciate the fact that I have gotten a chance to know executive leadership as well as providers in other departments. The ability to work together has allowed us to improve our projects and help push them forward. I have also had the opportunity to learn skills in quality improvement. I know that the work done through the FBCC will continue to enhance the medicine practiced at North Central Bronx Hospital” - Dr. Jana Romm, Pediatrics
The Pandemic is not over…but the FBCC continues!
Drs. Kaufman and Romm provided an overview of their experience at the first System Wide Collaboration Council meeting held after the first surge of the Pandemic in September, 2020. They shared their experience, summarized here:
● They decided to stop meeting during the height of the pandemic due to:
o Changes and disruptions in patient flow
o Re-deployment of staff
o Infection protection for group meetings
● They looked at their projects started before the surge
o Framed in the context of new work flows
o Kept in mind the possibility of another surge
o Wanted to keep the staff engaged
● Determinations made:
o Pausing is OK…not something to be seen as a setback
o The surge created its own Performance Improvement opportunities by showing the staff how to work differently and pivot more seamlessly
● Re-started pre-pandemic projects and created new post-surge projects in the following departments:
o Adult ED
o OB/GYN
o Dental
o Behavioral Health
o Peds ED
o Mobility Project in the Inpatient units
o Outpatient Pediatrics
In March, 2021, interviews were conducted with FBCC members including, Drs. Josephine Sullivan, Megan Bejtullah, Shellyann Sharpe, Chinyere Anyaogu, Jacinth Ruddock, Maninder Singh, Daran Kaufman, and Jana Romm. Their observations about work in the FBCC post-pandemic include:
● The doctors found ways to support each other through their collective improvement initiatives
● We learned how to expose staff to sicker patients
● The Quality Improvement tools and learning gave us a way to achieve qualitative analysis for data, especially in conjunction with PDSA cycles
● We developed successful ad hoc teams to deal with the COVID surge
● We learned of similar struggles that colleagues were having in other departments
● We formalized the idea of a true team, not one just run by executives
● We developed a new Collaborative Care program with social workers, psychiatrists, and nurses to help us screen patients and enhance our engagement with them; this helped get over the stigmas associated with referrals to behavioral health
● We confronted burnout head on: we asked ourselves together: “why do we do what we do”? This helped us when we “hit the wall” and we found energy from these discussions
● Instead of focusing on what is broken, we found the tools we needed through our dialogue
● We fixed problems that seemed insurmountable
● We have great executive support
Finally, let’s look in detail at one of the most recent projects of the FBCC undertaken since the pandemic surge:
Enrollment of patients in new electronic medical record systems is a critical challenge for health systems everywhere. This is especially true for Systems like NYC H + H that serve those patients in poor communities who are most challenged with communications. Integration of ALL patients’ primary care visits, biometrics, prescriptions, lab results, hospital stays into one electronic medical records system is one of the essential innovations in health care delivery that can improve health, reduce cost, and improve the patient experience.
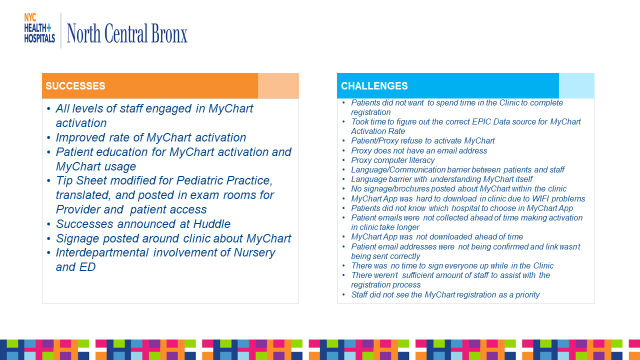
The MyChart Activation Improvement Project from the NCB FBCC is a truly great example of how frontline doctors and their managers can make direct and sustainable improvements. The full project charter is attached in the Appendix. Below are some of the achievements of the Project:
Today, Dr. Daran Kaufman is the Chief Medical Informatics Officer at NCB.
Dr. Jana Romm, an NCB staff pediatrician, continues her leadership role in the NCB FBCC.
In a recent interview, they shared their love of their work:
“People who work here want to work here; they bring a sense of community. Working in a challenging environment tends to unite people. We work in the shadow of the enormous resources of Montefiore which creates for us a healthy sense of competition.
Even though, “Monte” accepts the public health plan, MetroPlus, we believe our patients prefer to come to us at NCB.
While COVID brought tremendous stress, we cannot tell you how proud we were when the State tapped our little hospital to add 125 ICU beds to receive the overflow from much larger hospitals.
That’s why we love to call ourselves “the little hospital who could”.

Left to Right: MD Alam, IT director, Neena Phillips, CNO, Megan Bejtullahu, M.D. Jana Romm, M.D. Jacinth Ruddock, M.D, Chinyere Anyaogu, Deputy CMO , Janet Williams, CNM, Shellyann Sharpe, M.D., Josephine Sullivan, DDS, Nereida Correa, M.D. (not pictured, Daran Kaufman, MD,MBA and CMIO
Note on the authors:
John August is Program Director, Healthcare and Partner Programs, ILR Scheinman Institute, Cornell University
Samantha Na is Research Assistant, ILR Scheinman Institute, ILR student at Cornell University
Acknowledgment:
Sarah Chowdhury, Program Administrative Assistant, for her formatting and editing assistance
Appendix
Appendix 1: Final Contract Language
Appendix 2: QI Fundamentals
Appendix 3: MyChart QAPI
[i] “Patient Centered Collective Bargaining”, John August, ILR Scheinman Institute BLOG, April, 2021.
[ii] Trust for America’s Health website, May, 2021.
[iii] Scheinman Institute BLOG, April, 2021
[iv] “Building a Collaborative Community”, Paul Adler, Charles Heckscher, and Laurence Prusak, Harvard Business Review, July/August 2011.
[v] “Learning as the Foundation of Change,” Work and the Future, BLOG, John August, May 2021.
[vi] “Employee Engagement Drives Healthcare Quality and Financial Returns”, Rick Sherwood, Harvard Business Review, October 30, 2013
[vii] “Why does the quality of healthcare continue to lag?”, Nembhard, IM, Alexander, JA, Hoff, TJ, Ramanujan, R., Insights from Management Research: Academy of Management Perspectives, 2009; 23 (1): 24-42
[viii] Data from North Central Bronx Community Needs Assessment, 2013, 2016, 2019.
[ix] Quinones, Miriam; Moloney, Síle (6 May 2020). "New Covid-19 ICU Opens at North Central Bronx Hospital". Norwood News.
[x] Norwood, Christopher (August 23, 1982). Delivering babies the old fashioned way (New York Magazine ed.). New York Media, LLC. pp. 66–68.
